A recent study published in Complex Psychiatry indicates that individuals with a history of depression who consume high levels of caffeine report greater psychological distress. Researchers discovered genetic variations influencing both caffeine consumption and sensitivity to its effects. While caffeine intake did not show a strong correlation with sleep satisfaction, participants who indicated that caffeine affected their sleep typically consumed less of it. However, high doses of caffeine can exacerbate anxiety and disrupt sleep.
Previous research suggests that moderate caffeine consumption might lower the risk of developing depression in healthy individuals, but its impact on those already diagnosed remains less clear. Harry McIntosh, a PhD student at the University of Queensland and the study’s lead author, noted the increasing consumption of caffeine among younger populations and the rise in mental health issues, particularly insomnia, which is a symptom of various mental health disorders. “Caffeine could be a factor that individuals facing mental health challenges might adjust to improve their well-being and sleep,” McIntosh stated.
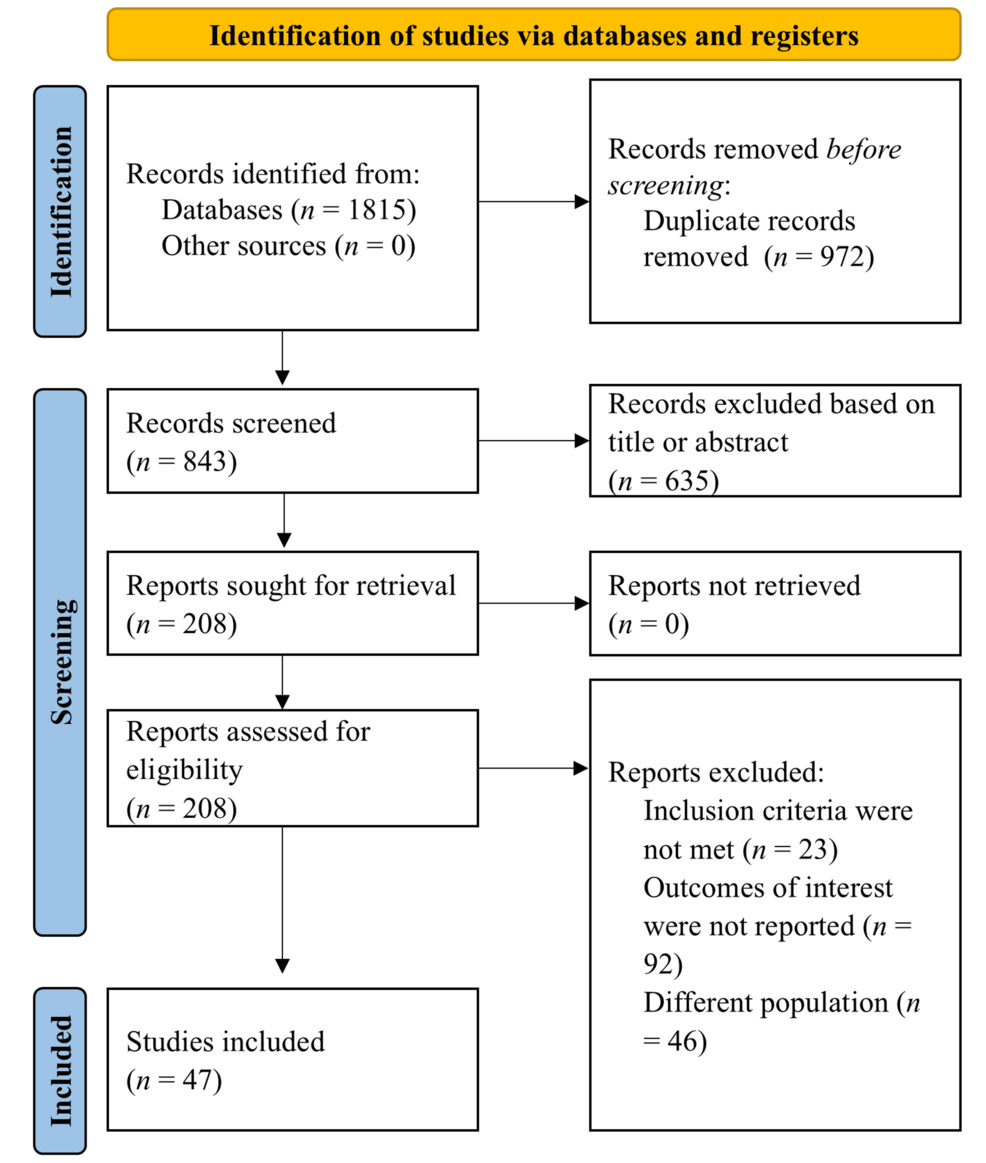
The study utilized data from the Australian Genetics of Depression Study, which involved over 11,000 adults diagnosed with or treated for depression. Participants completed detailed questionnaires regarding their caffeine habits, sleep quality, and mental health status. Approximately 9,000 participants also provided DNA samples, allowing researchers to link genetic differences to caffeine metabolism and sensitivity.
Caffeine consumption was categorized as low (0-2 drinks), medium (3-5 drinks), or high (6 or more drinks). Psychological distress was measured using the Kessler Psychological Distress Scale, a standard tool for assessing anxiety and depression symptoms. Sleep satisfaction was evaluated with a single item from the Insomnia Severity Index, and participants reported whether caffeine interfered with their sleep, indicating sensitivity.
Using linear regression models, researchers examined the relationship between caffeine intake, psychological distress, and sleep satisfaction while controlling for factors such as age, sex, body mass index, and other substance use (including alcohol, nicotine, and painkillers). The analysis revealed that individuals consuming six or more caffeinated drinks daily reported higher distress scores compared to those with lower consumption. For each additional caffeinated beverage consumed per day, distress scores increased by 0.2 points on a 50-point scale. Although this effect was small, it was statistically significant. The medium caffeine group (3-5 drinks per day) did not exhibit significant differences from the low group, indicating that only higher caffeine consumption correlates with increased distress.
Interestingly, caffeine intake did not appear to adversely affect sleep satisfaction among participants. Those with higher caffeine consumption reported slightly lower sleep satisfaction, but this difference was minimal and not statistically significant after adjusting for multiple comparisons. McIntosh explained that caffeine sensitivity seemed to play a larger role; individuals who reported caffeine disrupting their sleep were less likely to consume large amounts. Each additional caffeinated drink consumed daily was associated with a 16% lower chance of reporting caffeine sensitivity, suggesting people may naturally limit their intake if they notice a negative impact on sleep.
Genetic analysis revealed several variants linked to differences in caffeine consumption. For instance, a variant near the AHR gene (rs4410790) correlated with higher caffeine intake, while a variant near the CYP1A2 gene (rs2472297) was associated with lower consumption. These genes influence caffeine metabolism, meaning faster metabolizers may consume more to achieve the same alertness level, whereas slower metabolizers may limit their intake. Another variant near the MMS22L/POU3F2 genes (rs34645063) indicated a higher likelihood of reporting caffeine sensitivity, aligning with previous findings that lower caffeine consumption is linked to increased sensitivity. Other variants in genes like ADORA2A, which encodes a caffeine-targeted receptor in the brain, showed weak links to consumption and lost significance after multiple comparisons.
McIntosh emphasized that their research focused on individuals diagnosed with depression, finding a correlation between higher caffeine consumption and increased stress levels, regardless of sleep quality. While the effect size was small, it was statistically significant. However, the study cannot establish causation, as participants might consume more caffeine in response to depressive symptoms such as fatigue or lack of motivation. Genetic variants significantly influence how individuals metabolize caffeine and their consumption levels.
One major strength of the study is its large sample size and genetic data inclusion, allowing the detection of even minor effects. Nonetheless, the cross-sectional nature of the data captures only a single time point, making it difficult to ascertain cause-and-effect relationships. McIntosh noted, “Our data reflects only one moment and measures variables rather than controlling them experimentally, so we cannot definitively state that caffeine is causing distress or that those with higher distress are consuming more caffeine.”
Another limitation is that the study’s sample consisted entirely of people with a history of depression, which may not be representative of the general population, particularly those without mental health conditions. Future research with more precise caffeine intake measurements and longitudinal designs could clarify these relationships over time.