Bipolar disorder (BD) affects approximately 1% of the global population, characterized by alternating manic and depressive episodes. While effective medications exist to alleviate symptoms, challenges such as treatment resistance and the need for ongoing therapy persist. Current diagnostic and treatment approaches often focus on symptoms rather than underlying biological causes, highlighting the need for a deeper understanding of BD’s biological mechanisms.
Recent research has utilized single-molecule DNA analysis to investigate the role of brain mitochondria in BD. Mitochondria are essential for energy production and calcium regulation in neurons, and dysfunctions in these organelles have been linked to various neuropsychiatric disorders. Studies indicate that patients with BD exhibit mitochondrial abnormalities, such as damage to mitochondrial proteins due to oxidative stress.
Genomic studies have shown that BD has a high heritability rate, prompting researchers to explore its genetic architecture. Large-scale genome-wide association studies have identified links between BD and genes involved in synaptic function and fatty acid metabolism. Some studies have also pointed to copy number variations and de novo mutations in certain genes as potential risk factors for BD.
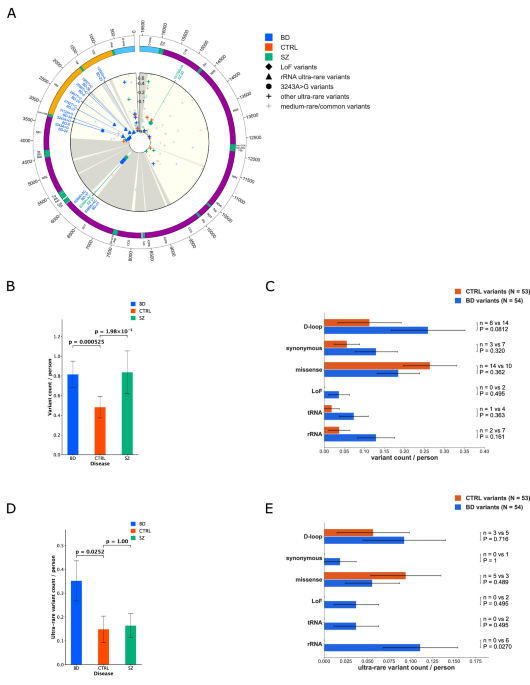
A notable finding from this research is the association between mitochondrial DNA (mtDNA) variants, particularly heteroplasmic variants, and BD. Heteroplasmy refers to the presence of multiple mitochondrial DNA types within a single cell. The study revealed an enrichment of specific mitochondrial variants, including the m.3243A>G variant, in postmortem brain samples from BD patients. This variant, known for its role in mitochondrial diseases like MELAS (mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes), was found alongside other mutations related to rRNA and tRNA genes.
The researchers conducted a thorough analysis of 163 postmortem brain DNA samples, comparing those from BD patients with samples from healthy controls and patients with schizophrenia. The study specifically focused on two models of association between BD and mitochondrial heteroplasmic variants: one involving pathogenic variants that impair neural functions and another addressing the accumulation of numerous low-level heteroplasmic variants.
Results from the analysis showed that while BD patients had a higher number of high-variant allele fraction (VAF) heteroplasmic variants compared to controls, there was no significant increase in low-level heteroplasmic variants. This suggests that specific pathogenic variants may play a more critical role in BD than previously understood.
The findings of this study underline the necessity of understanding the genetic and biochemical underpinnings of BD to develop targeted therapies. Mitochondrial variant profiles could inform future treatment strategies, potentially leading to more effective interventions for patients struggling with bipolar disorder. The research, which adheres to ethical guidelines and received approval from relevant ethics committees, paves the way for further exploration of mitochondrial genetics in mental health conditions.